What Is Chronic Dry Eye Syndrome?
- Dr. Zimski
- Feb 15, 2024
- 5 min read
Updated: May 29, 2024
Tears are critical for eye health. They wash away foreign objects, protect against infection, and lubricate the surface of your eyes. When your tears aren’t doing their job, you can experience a scratchy feeling, constant dryness, and stinging eyes.
Dry eyes can make reading, working on the computer, or any activity that requires sustained visual attention more difficult.
The condition can make wearing contact lenses more trouble than it’s worth.
Other names for dry eye include keratoconjunctivitis sicca (KCS), evaporative dry eye, aqueous tear deficiency, and neurotrophic keratitis.

Symptoms of Chronic Dry Eye
Chronic dry eye is most often characterized by a dry, gritty or burning sensation in the eyes. Other common symptoms of dry eye syndrome include:
Blurred vision
Red eyes
Heavy eyelids/eyes that that are hard to open after sleeping due to stickiness
Feeling like something is in your eye
Eyestrain
Fatigued or sore eyes
Itchy eyes
Light sensitivity (photophobia)
Stinging eyes
Discharge from the eye
Inability to cry
Many of our patients find this strange, but watery eyes also can be a symptom of dry eye syndrome! This is because your eyes (in response to dryness on the eye’s surface) can over-produce the watery component of your tears as a protective mechanism. “Reflex tears” don’t stay long enough to correct the underlying dry eye condition.
What Causes Dry Eye?
An adequate layer of tears on the surface of the eye is essential to keep them healthy, comfortable and functioning. The “tear layer” keeps the eye’s surface moist, protecting it from environmental damage. The tear layer keeps the cells and glands of the eye healthy and functioning.
Without a consistently adequate layer of this tear layer, you’re at risk of corneal nerve damage, eye infection, and chronic dry eye.
But it turns out there’s more to your tears than meets the eye …
In fact, normal tear film consists of three important components, each serving a critical purpose:
An oily/lipid component increases lubrication and help keep the tear film from evaporating too quickly
A watery (aqueous) component lubricates the eye, washes away particles and prevents infection.
A mucous-like (mucin) component helps anchor and spread the tears across the surface of the eye
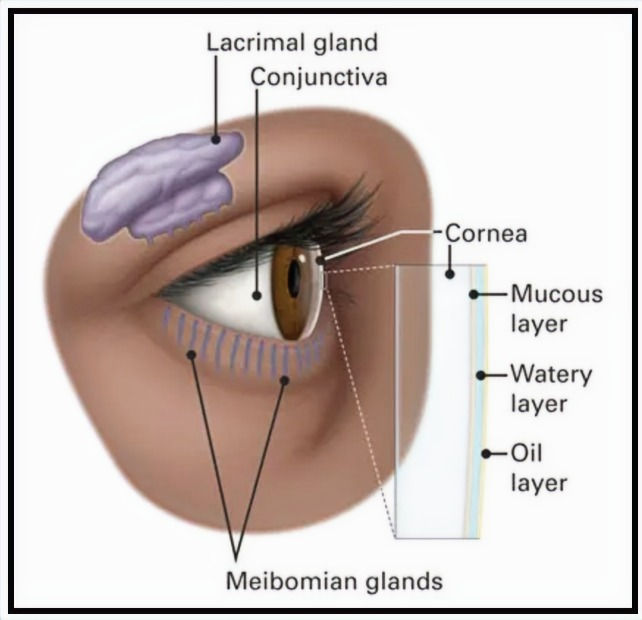
Courtesy American Academy of Ophthalmology
Each tear film component is produced by different glands on or near the eye:
Meibomian glands in the eyelids produce the oily/lipid component.
Lacrimal glands (behind the outer aspect of the upper eyelids) produce the watery component (aqueous)
Goblet cells in the conjunctiva that covers the white of the eye (sclera) produce the mucin component.
A problem with any of these glands can cause dry eyes.
To make things a tad more complicated, there are different categories of dry eyes, depending on which component is affected.
For example, evaporative dry eye is when the meibomian glands don’t produce or secrete enough oil (meibum), causing the tear film to evaporate too quickly. The underlying condition — meibomian gland dysfunction — is recognized as a significant factor in many cases of dry eye syndrome.
Another condition, aqueous deficiency dry eye, is when the lacrimal glands fail to produce enough watery fluid to keep the eyes adequately moistened.
The specific type of dry eye often will determine the type of treatment you need. See our article about Lumenis Laser Treatment to learn about one of the most effective procedures for treating chronic dry eye.
Other Factors That Lead To Chronic Dry Eye
Dry eyes can develop for many reasons, including:
Screen time – the incidence and severity of dry eye increases with extended screen time. Computer over-use leads to decreased blinking and eye stress.
Natural aging or hormonal changes (women over 50 are particularly susceptible to dry eye disease, or DED)
Cosmetic surgery (e.g. if the eyelids are opened too widely)
Certain medications, like antihistamines and blood pressure drugs
Medical conditions like diabetes, blepharitis, and lupus
Extended use of contact lenses or conditions that affect eyelid closure
People with specific medical conditions are at a higher risk, such as autoimmune disease like Sjogren’s. With thyroid eye disease (when the eye protrudes forward), there is often an increase in the surface of the eye, leading to increased issues with adequate tear production.

What Are The Dangers Associated With Dry Eyes?
Decreased tears lead to the tears being too salty (hyperosmolarity), instability and inflammation and they all tend to co-exist. This tear film disturbance affects cells on the surface of the eye and triggers the inflammatory cascade.
As dry eye disease (DED) progresses, so does the inflammation, and it damages the surface epithelium, nerves, and goblet cells, worsening the DED. Inflammation also results in changes in the meibomian glands (MGs) and MGD further perpetuates the cycle of DED.
Eventually, DED becomes an irreversible chronic inflammatory condition that is self-perpetuating, concurrent with a similar self-perpetuating vicious cycle of inflammation. In these conditions, DED is the initiating event and triggers inflammation. Chronic dry eye is driven by a vicious cycle of inflammation.
What Is The Difference Between Dry Eye And Chronic Dry Eye?
Temporary dry eyes can be caused by a dry climate or over-wearing contact lenses. Denver has dry air year-round due to the higher altitudes, so the issue is common here.
Chronic dry eye is a medical condition that, over time, can decrease the eye's ability to make and/or maintain sufficient quality and quantity of tears for a healthy tear film.
How do you know if your dry eye is chronic?
With chronic dry eye syndrome, the symptoms are more persistent. Severe cases can include light sensitivity, severe eye pain or changing vision. Anyone experiencing these symptoms should book an appointment and be properly diagnosed.
How Do We Treat Chronic Dry Eye?
Dry eye is a complex disease and unfortunately, there is no one-size-fits-all treatment approach that is effective, often leaving patients feeling frustrated.
A thorough exam is needed to evaluate all the factors that contribute to dry eye and then a tailored treatment approach can be recommended. This involves looking at the eyelid position, blink patterns, signs of facial and ocular rosacea, conjunctivochalasis, meibomian gland structure, oil composition and quantity, and tear “break up” time.
“In addition to the eye findings, a holistic approach is needed to treat the whole person,” says Dr. Lauren Zimski. “There are many factors outside of the eye that affect tear production, such as the environment, stress, anxiety, lack of sleep and too much screen time. All of these contribute to dry eye.”
The parasympathetic (rest and digest) nervous system is responsible for inducing tear secretion. Studies have shown that deep abdominal breathing increases tear production and simple exercises can be effective in helping decrease stress and increase tears.
Dry Eye Syndrome: Conclusion
Diagnosing dry eye disease requires a comprehensive eye exam, including a discussion of your symptoms and tests to evaluate tear quality and quantity. These tests help us determine the root cause of your dry eyes and tailor the best treatment plan for you.
Treatments can include lifestyle modifications, blinking exercises, treatment of demodex, eye drops to control inflammation, medications to stimulate the parasympathetic nervous system, Intense pulsed light (IPL) therapy, LipiFlow, gland expression, gland probing, oral medications for nerve pain, and more.
Don't let chronic dry eye syndrome diminish the quality of your daily life. Schedule a dry eye consultation with Dr. Zimski, where she will evaluate which treatment options are right for your unique symptoms. We can offer relief and restore eye comfort. Simply schedule your first appointment online, or contact us with any questions using our online form. Need more ways to get in touch? Try calling 303-863-1231.
